Healthcare organizations face unique scheduling challenges due to 24/7 operations, complex staffing requirements, and the critical nature of patient care. Mobile and digital scheduling tools have emerged as powerful solutions to these challenges, offering flexibility, automation, and improved communication capabilities. Implementation case studies from various healthcare settings demonstrate how these technologies can transform workforce management while improving both staff satisfaction and patient outcomes. From large hospital systems to small clinics, organizations that have embraced digital scheduling tools report significant operational improvements, cost savings, and enhanced quality of care.
This comprehensive guide examines real-world examples of healthcare facilities that have successfully implemented mobile and digital scheduling solutions. By analyzing these case studies, healthcare administrators can understand the challenges, benefits, and best practices associated with digital transformation in staff scheduling. The experiences of these organizations provide valuable insights into implementation strategies, change management approaches, and measurable outcomes that can be achieved through modern healthcare scheduling solutions. These lessons learned can help other facilities chart their own path toward more efficient, effective workforce management.
The Transformation of Healthcare Scheduling Through Digital Tools
The traditional methods of healthcare staff scheduling – paper schedules, spreadsheets, and manual processes – have become increasingly inadequate in today’s complex healthcare environment. Digital scheduling tools offer sophisticated capabilities that address the unique challenges faced by healthcare organizations. These tools have revolutionized how medical facilities manage their workforce through automation, mobile accessibility, and data-driven insights. According to research from healthcare technology consultants, facilities implementing digital scheduling solutions report up to 70% reduction in scheduling administration time and significant improvements in staff satisfaction scores.
- Complexity Management: Digital tools efficiently handle complex scheduling requirements including credentials, certifications, skill matching, and compliance with labor regulations.
- Real-Time Adjustments: Real-time schedule adjustments capabilities allow managers to quickly respond to call-offs, emergencies, or unexpected patient volume changes.
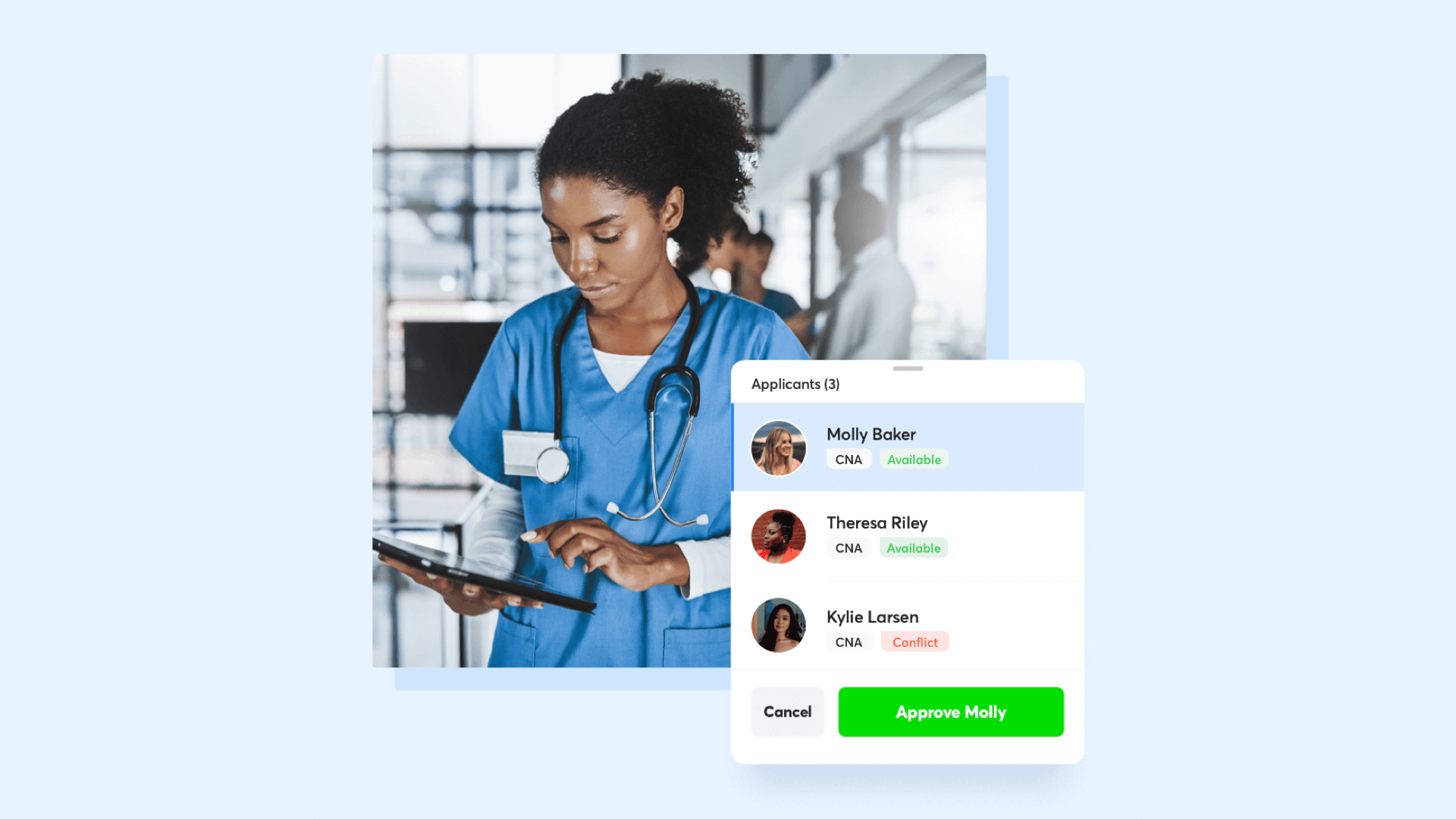
- Self-Service Features: Staff can view schedules, request time off, and swap shifts directly from their mobile devices, increasing autonomy and satisfaction.
- Interoperability: Modern solutions integrate with EHR systems, time and attendance, and payroll platforms for streamlined operations.
- Data-Driven Insights: Advanced analytics help administrators optimize staffing levels, forecast needs, and identify opportunities for efficiency improvements.
The transition to digital scheduling has become a strategic priority for healthcare organizations seeking to optimize operations while addressing staff burnout and turnover. According to a recent survey of healthcare administrators, 83% identified scheduling modernization as a critical factor in their workforce retention strategy. Successful implementations, as shown in the following case studies, demonstrate that mobile scheduling apps and digital platforms can transform healthcare operations when properly deployed with attention to change management and staff engagement.
Case Study 1: Major Metropolitan Hospital System Implementation
A major hospital system with eight facilities and over 15,000 staff members faced significant challenges with staffing inconsistencies, excessive overtime costs, and high turnover rates. Their legacy scheduling system required manual intervention, created communication gaps, and lacked mobile capabilities. In 2021, they implemented a comprehensive digital scheduling solution with mobile access, integrated communication features, and advanced analytics. The 18-month implementation was phased by department, beginning with nursing units, followed by ancillary departments and administrative staff.
- Implementation Strategy: Used a pilot program approach with champions from each department before full-scale deployment across all facilities.
- Integration Complexity: Successfully connected the scheduling platform with HR, payroll, and EHR systems to create a unified workflow.
- Change Management: Conducted over 200 training sessions and created role-specific guides to ensure staff adoption across all shifts and departments.
- Credential Tracking: Implemented healthcare credential tracking functionality to automatically flag certification expirations and ensure compliance.
- Analytics Dashboard: Deployed custom reporting tools for executives to monitor staffing metrics and labor costs across all facilities.
The results were significant and measurable: overtime expenses decreased by 18% within the first year, saving approximately $4.2 million annually. Nurse satisfaction scores related to scheduling increased by 23 percentage points, and time spent on schedule creation was reduced by 60% for unit managers. The hospital also reported a 15% reduction in agency staffing costs through improved internal resource allocation. “The mobile access was a game-changer for our staff,” noted the Chief Nursing Officer. “Being able to check schedules, request swaps, and communicate with their teams directly from their phones transformed how our teams collaborate and significantly improved work-life balance.” The hospital’s healthcare implementation case study has been featured in several healthcare management publications as a model for digital transformation.
Case Study 2: Multi-Location Ambulatory Care Network
A network of 12 ambulatory care centers serving over 250,000 patients annually struggled with inconsistent scheduling practices across locations, leading to patient wait times, underutilized resources, and staff dissatisfaction. Their previous system lacked coordination between facilities, making it difficult to optimize provider coverage and respond to fluctuating demand. In 2022, they implemented a cloud-based scheduling solution specifically designed for ambulatory settings with integrated patient flow forecasting capabilities.
- Cross-Location Coordination: Implemented a system that enabled healthcare multi-location scheduling to distribute providers across sites based on patient volume predictions.
- Skills Database: Created a comprehensive provider skills database to ensure appropriate coverage for specialized services at each location.
- Mobile Accessibility: Deployed mobile apps that allowed providers to view schedules, request changes, and receive notifications about coverage needs.
- Demand Forecasting: Utilized historical data and seasonal trends to predict staffing needs and adjust schedules accordingly.
- Provider Preferences: Incorporated physician and staff scheduling preferences while maintaining equitable distribution of desirable and less-desirable shifts.
The implementation yielded impressive results over an 8-month period. Patient wait times decreased by 32% across all locations, while provider utilization improved by 27%. The network experienced a 40% reduction in last-minute schedule changes and a 35% decrease in overtime costs. The ability to float providers between locations based on demand resulted in more balanced workloads and improved access to care. “The mobile scheduling solution has transformed our ability to adapt to changing circumstances,” said the network’s Operations Director. “When we have unexpected provider absences or patient volume spikes, we can quickly identify and deploy available resources from other locations.” This successful implementation demonstrates how mobile schedule access can enhance operational agility across multiple facilities while improving both provider satisfaction and patient experience.
Case Study 3: Long-Term Care Facility Staffing Transformation
A chain of five long-term care facilities with 450 beds and 300+ staff members faced chronic staffing challenges, including high turnover rates (exceeding 40% annually), inconsistent coverage, and difficulty complying with resident-to-staff ratio requirements. Their paper-based scheduling system created communication gaps that frequently led to understaffing and excessive agency usage. In 2020, they implemented a specialized digital scheduling solution with shift swapping capabilities and mobile access for all staff members.
- Self-Service Portal: Implemented a staff portal allowing caregivers to view schedules, request time off, and swap shifts from any device.
- Compliance Tracking: Built-in compliance monitoring ensured that staffing ratios met state regulations and tracked required staff certifications.
- Shift Bidding System: Created a shift marketplace where open shifts could be posted and staff could bid on preferred assignments.
- Communication Platform: Integrated messaging tools allowed managers to instantly notify qualified staff about open shifts and emergent needs.
- Automated Alerts: System generated notifications about potential understaffing or compliance issues before they became problems.
The results were transformative for the organization. Within one year, staff turnover decreased from 42% to 28%, resulting in savings of approximately $780,000 in recruitment and training costs. Agency staffing usage decreased by 60%, saving an additional $1.2 million annually. The facilities achieved 98% compliance with staffing regulations, up from 82% pre-implementation. “Our staff feel empowered by having more control over their schedules,” noted the HR Director. “The ability to swap shifts or pick up additional hours through the mobile app has dramatically improved both satisfaction and retention.” The implementation of healthcare staff scheduling technology created a virtuous cycle where improved staffing levels led to better patient care, which further enhanced staff satisfaction and retention. This case demonstrates the significant return on investment possible when digital scheduling tools address the specific needs of long-term care environments.
Case Study 4: Rural Hospital Scheduling Modernization
A 125-bed rural hospital serving a large geographic area faced unique staffing challenges, including limited local workforce, extreme weather disruptions, and the need to maintain essential services with minimal staff. Their outdated scheduling system required manual intervention, creating inefficiencies and often resulted in either overstaffing or dangerous understaffing situations. In 2021, they implemented a cloud-based scheduling platform with healthcare shift planning capabilities designed for rural healthcare settings.
- Contingency Planning: Built-in features for weather emergencies and disaster scenarios to quickly identify essential personnel and backup staff.
- Cross-Training Tracking: System tracked staff with multiple competencies to maximize flexibility during staffing shortages.
- Mobile Communication: Push notifications and text alerts ensured staff awareness of schedule changes even in areas with limited connectivity.
- Fatigue Management: Algorithms prevented unsafe scheduling patterns for staff working extended hours during emergencies.
- Integration with EHR: Connected scheduling with patient census data to dynamically adjust staffing based on actual patient needs.
The implementation yielded remarkable improvements in the hospital’s operations. Staff satisfaction scores increased by 26%, while overtime costs decreased by 22% in the first year. The hospital reduced reliance on traveling nurses by 30%, resulting in annual savings exceeding $500,000. During a major winter storm, the system allowed rapid deployment of an emergency staffing plan, ensuring continuous patient care despite 40% of staff being unable to travel to the facility. “The mobile scheduling solution transformed our ability to respond to rural healthcare challenges,” explained the Chief Operating Officer. “Staff now have real-time visibility into schedules and can communicate availability changes instantly, which has been particularly valuable during emergency situations.” This case demonstrates how digital scheduling solutions can be tailored to address the unique challenges faced by rural healthcare providers while improving both operational resilience and financial sustainability. The implementation of healthcare implementation examples like this one has become a model for other rural facilities facing similar challenges.
Implementation Challenges and Solutions in Healthcare Settings
While the benefits of digital scheduling solutions in healthcare are substantial, implementation is not without challenges. The case studies reveal common obstacles that healthcare organizations faced during their digital transformation journeys. Understanding these challenges – and the strategies successful organizations used to overcome them – can help other healthcare facilities prepare for their own implementations. Many organizations discovered that technical issues were often easier to resolve than cultural and procedural challenges related to change management.
- Resistance to Change: Many healthcare organizations reported initial staff resistance, particularly among long-tenured employees accustomed to traditional methods.
- Legacy System Integration: Connecting new scheduling platforms with existing HR, payroll, and EHR systems created technical hurdles for IT teams.
- Compliance Concerns: Ensuring the new systems maintained compliance with healthcare worker regulations, union contracts, and internal policies required careful configuration.
- Training Constraints: Providing adequate training across all shifts and departments without disrupting patient care proved logistically challenging.
- Data Migration Issues: Transferring historical scheduling data, staff preferences, and credentials from legacy systems required significant planning and validation.
Successful implementations addressed these challenges through comprehensive strategies. Organizations that thrived established clear governance structures with executive sponsorship and identified department-level champions. They created phased implementation plans aligned with implementation timeline planning best practices, starting with pilot departments before expanding. Many facilities developed multi-modal training approaches including in-person sessions, online modules, and reference materials accessible via mobile devices. Communication plans emphasized the benefits to both staff and patients, focusing on how the new tools would solve existing pain points rather than simply introducing new technology. As one Nursing Director noted: “We succeeded because we made this about improving work-life balance for our nurses, not just about implementing new software.”
Key Benefits Revealed in Healthcare Scheduling Case Studies
The collective results from the case studies reveal consistent benefits that healthcare organizations achieved through digital scheduling implementations. These outcomes demonstrate the substantial return on investment possible when healthcare facilities implement comprehensive mobile and digital scheduling solutions. While the specific metrics varied across different organization types and sizes, patterns emerged showing improvements in operational efficiency, financial performance, staff experience, and ultimately patient care quality.
- Cost Reduction: Organizations consistently reported 15-30% decreases in overtime costs and agency staffing expenses through improved schedule optimization.
- Time Savings: Administrative time spent on scheduling decreased by 50-70% across organizations, freeing managers to focus on patient care and staff development.
- Improved Compliance: Facilities achieved 95-99% compliance with regulatory requirements, reducing risk of penalties and ensuring proper healthcare credential compliance.
- Enhanced Communication: Organizations reported 40-60% reductions in scheduling-related communication issues and conflicts.
- Staff Retention: Turnover rates decreased by 10-25% among organizations that implemented digital scheduling with self-service capabilities.
Beyond these quantitative benefits, healthcare organizations reported qualitative improvements including enhanced work-life balance for staff, increased transparency in scheduling decisions, and greater organizational agility during crisis events. The implementation of healthcare shift handovers features in digital platforms also improved continuity of care between shifts. “The ROI extends beyond direct cost savings,” explained one CFO. “When our staff are less stressed about schedules and can access them easily on their phones, they bring better energy to patient interactions, which ultimately impacts our patient satisfaction scores.” Healthcare leaders emphasized that while the initial investment in digital scheduling technology was significant, the return typically materialized within 12-18 months through hard cost savings alone, with ongoing benefits accumulating over time.
Best Practices for Healthcare Scheduling Implementation
Analysis of successful healthcare scheduling implementations reveals a set of best practices that significantly increase the likelihood of positive outcomes. Organizations that achieved the greatest benefits from their digital scheduling transformations consistently followed certain approaches throughout their implementation journeys. These practices address the unique challenges of healthcare environments while maximizing staff adoption and system effectiveness. Healthcare leaders considering similar implementations should incorporate these lessons learned into their planning process.
- Stakeholder Engagement: Include representatives from all affected roles—from executives to frontline staff—in the selection and implementation planning process.
- Thorough Needs Assessment: Conduct comprehensive analysis of current scheduling challenges, workflow inefficiencies, and specific departmental requirements before selecting a solution.
- Future-Focused Selection: Choose platforms with mobile technology capabilities that can grow with the organization and adapt to evolving healthcare delivery models.
- Phased Implementation: Start with pilot departments that have strong leadership and receptive staff before expanding to more complex areas.
- Comprehensive Training: Develop role-specific implementation and training programs accessible across all shifts and user comfort levels with technology.
Organizations that achieved the greatest success devoted significant resources to change management, recognizing that technology alone cannot transform operations without corresponding adjustments to processes and culture. They established clear metrics for success before implementation and regularly measured progress against these benchmarks. Successful implementations also maintained strong relationships with their technology vendors, treating them as strategic partners rather than just service providers. “We created a continuous feedback loop between our staff, our internal project team, and our technology provider,” shared one Chief Nursing Informatics Officer. “This allowed us to quickly identify and address issues before they became significant barriers to adoption.” By following these best practices and learning from the experiences documented in these case studies, healthcare organizations can maximize the return on their investment in digital scheduling solutions while minimizing disruption to their operations.
Future Directions: Evolution of Healthcare Scheduling Technology
The case studies examined not only demonstrate current benefits but also point toward emerging trends in healthcare scheduling technology. Organizations that have successfully implemented digital scheduling solutions are now exploring advanced capabilities to further enhance their operations. These forward-looking organizations are partnering with technology providers to shape the next generation of workforce management tools specifically designed for healthcare environments. Understanding these trends can help healthcare leaders make strategic technology decisions that will remain relevant as the industry evolves.
- AI-Powered Optimization: Advanced algorithms that incorporate machine learning to improve scheduling accuracy based on historical patterns and real-time factors.
- Predictive Analytics: Tools that forecast patient volumes and acuity to proactively adjust staffing levels before shortages occur.
- Staff Wellness Integration: Scheduling systems that factor in fatigue management, work-life balance preferences, and burnout prevention strategies.
- Cross-Departmental Coordination: Enhanced capabilities for cross-department schedule coordination to optimize care team composition across disciplines.
- Patient-Centered Scheduling: Integration of staff scheduling with patient appointment systems to ensure optimal alignment of resources.
Many organizations in the case studies are exploring the integration of artificial intelligence and machine learning into their scheduling processes. For example, one hospital system is piloting an AI-driven system that predicts patient surge events 24-48 hours in advance, allowing proactive staff adjustments. Another organization is testing natural language processing to enable voice-based schedule inquiries and shift swaps through mobile devices. “The future of healthcare scheduling isn’t just about automation – it’s about intelligent anticipation of needs,” explained one Chief Digital Officer. “We’re moving from reactive to proactive workforce management through these advanced technologies.” As healthcare continues to face staffing challenges and increasing patient demands, these emerging technologies will play a crucial role in creating sustainable, efficient scheduling solutions that support both operational excellence and staff wellbeing.
Measuring ROI: Quantifying the Impact of Digital Scheduling
For healthcare executives considering investments in digital scheduling solutions, understanding the potential return on investment is crucial. The case studies provide valuable insights into how organizations have measured and quantified the benefits of their implementations. While some benefits were immediately visible in financial terms, others manifested as operational improvements, risk reduction, or staff experience enhancements. Developing a comprehensive ROI framework before implementation helps organizations track progress and justify continued investment in scheduling technology.
- Direct Cost Reduction: Organizations tracked savings from reduced overtime, agency staffing, and administrative hours devoted to scheduling tasks.
- Productivity Gains: Facilities measured increased patient-facing time for clinical staff and more efficient unit operations through better scheduling.
- Risk Mitigation: Improvements in compliance rates and reductions in scheduling-related incidents were quantified and valued.
- Retention Impact: Organizations calculated the financial impact of reduced turnover, including recruitment, onboarding, and training cost avoidance.
- Quality Metrics: Some facilities linked scheduling improvements to patient satisfaction scores and clinical quality measures through reporting and analytics.
Healthcare organizations found that building a comprehensive business case that included both quantitative and qualitative benefits was essential for securing leadership support and sustaining momentum through implementation challenges. One community hospital created a balanced scorecard approach to track their digital scheduling implementation, measuring financial outcomes alongside staff experience, operational efficiency, and patient impact metrics. “We initially f